Tubal Ligation Reversal
Your Tubal Reversal Surgeon
Dr. Shane Lipskind has been performing tubal ligation reversals since training in advanced laparoscopic and microsurgical techniques as a reproductive endocrinology and infertility (REI) fellow. He has performed hundreds of tubal ligation reversals for his patients with extremely high rates of success.
Dr. Lipskind uses an operating microscope or the daVinci surgical robot to perform all of his end-to-end tubal microanastomoses. He prefers to use the operative microscope in most cases because it can magnify the operative field many more times than surgical loops or the robotic laparoscope, and thus provides better visualization so that extremely small sutures can be used to reunite the fallopian tubes. Because he uses permanent sutures so small they’re barely visible to the naked eye, there is virtually no inflammatory response from the surrounding tissue, and the risk of tubal re-occlusion or scar tissue-induced ectopic pregnancy are drastically reduced.
Due to his meticulous technique, Dr. Lipskinds rates of tubal patency after microanastomosis exceed 90%, which means that your tubes are highly likely to remain open. Pregnancy and live birth rates after successful microanastomosis are then dependent upon the age of the female partner and the couple’s natural fertility. This is why some basic testing, including ovarian reserve testing and semen analysis, are recommended prior to tubal reversal. Fertile women under the age of 35 can expect greater than an 80-85% chance of having a child within two years of the surgery. Although ACFS always counsels extensively regarding the risk of ectopic pregnancy after any tubal surgery, tubal pregnancy affects fewer than 5% of patients who become pregnant after tubal reversal at our center.
“Can my tubal ligation be reversed?”
Patients often worry that their tubal sterilization cannot be reversed if they have had their tubes cut, tied, burned (cauterized), or any combination of the three. Although some tubal sterilizations are easier to reverse than others (Filshie clips, Hulka clips, and Falope rings), it actually does not matter how your sterilization was done. The most important factor is the length of the tubal segments that were left unharmed. A full-length fallopian tube measures 8-12 centimeters long, and most sterilization procedures remove or damage 2-5 cm of the tube. We want our patients to have greater than 4 cm of tubal length remaining so that the newly repaired tubes will function as they should and provide an excellent chance for pregnancy. For these reasons, we always make an effort to obtain operative reports from the tubal ligation surgery when they are available. Sometimes, unfortunately, the operative reports reveal that the fallopian tube was removed or destroyed in its entirety. Learning this ahead of time can save you a disappointing and needless trip to the operating room. In most cases, however, the operative reports will reassure us that the odds of being able to complete your tubal ligation reversal are high.
In addition to obtaining the prior surgical records, we also perform a diagnostic laparoscopy at the start of every reversal surgery to confirm that there is enough healthy tube remaining. Operative reports do not always match what was actually done or the current status of the tubes because inflammation and scarring during the healing process can do additional damage after the tubal ligation itself. To do the laparoscopy, we make a tiny incision in the belly button and insert a long, thin camera into the abdomen to look directly at the fallopian tubes. Approximately 90% of the time, this will confirm that we can do the reversal.
Some clinics recommend a hysterosalpingogram (HSG) to see if there is enough tubal length prior to the surgery. The problem with HSG is that it only hints at how much tubal segment there is up to the point where the tube was “tied.” It cannot expose how much tubal length remains beyond that point. This can mislead us to believe that there is not enough tube remaining if the tubes were tied close to the uterus, or that it will be an easy reversal when the second half of the tube may have been completely removed or destroyed. Therefore, we do not use HSG to determine whether a patient is a candidate for a tubal reversal.
How is Tubal Micro-anastomosis Performed?
First, your anesthesiologist will make sure that you are asleep and comfortable in the operating room. Then, a catheter will be placed into the uterus to allow for injection of a sterile blue dye to show that the fallopian tubes are open after completion of the repairs. A small incision is then made in the belly button, and the abdomen is inflated with CO2 gas. The laparoscope will be inserted into the abdomen to visualize the fallopian tubes. When it is confirmed that a reversal can be performed, a small bikini incision (mini-laparotomy) of less than 2.5 inches is made right above the pubic bone. Once access to the fallopian tubes is established, new tubal openings are created, and the operating microscope brought into position. The tubes are then reunited using microsurgical technique and approximately 4 sutures for the inner layer of each tube and 10 sutures for the outer layer, or serosa. The blue dye is injected when the anastomoses, or re-joining of the tubes, are complete, confirming that the dye spills freely from the end of the tubes and that the repair sites are water-tight. Upon completion of the anastomoses, the abdominal incision is closed in layers. The skin incision is closed with absorbable suture. Anesthesia is then reversed, and you are taken to the recovery area for observation.
Tubal Reimplantation
If your tubal ligation was performed too close to where the tubes attach to the uterus, then you will not be a candidate for an end-to-end tubal microanastomosis. You may, however, be a candidate for tubal reimplantation, a procedure in which a new opening is made in the uterus and the distal fallopian tube is inserted. The fallopian tubes are held in place by a stent that is removed three months later in the office.
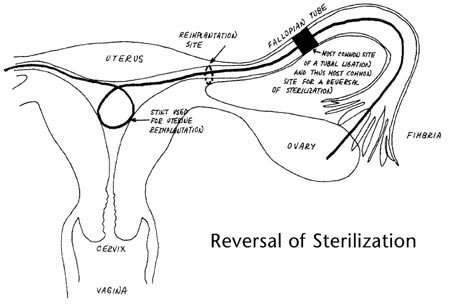
Although tubal reimplantation surgery can be an effective technique, it is important to note that tubal patency rates and pregnancy rates are lower than the more common end-to-end anastomosis (approximately 50-60% tubal patency after reimplantation vs. over 90% for traditional reversal). In addition, patients undergoing tubal reimplantation must allow three months of uterine healing time before attempting pregnancy and will be required to deliver by c-section.
How Long Does Tubal Reversal Surgery Take?
The actual procedure takes 2-3 hours, and you can go home the following morning.
Is Tubal Reversal Surgery Performed Under Anesthesia?
The surgery is performed under general anesthesia so that you are completely asleep and comfortable throughout the procedure.
Risks Associated With a Tubal Ligation Reversal
Complications from tubal reversal surgery are rare. The procedure is less risky than a c-section and carries about the same risk as a tubal ligation. Operative risks shared by all forms of abdominal surgery include bleeding, infection, injuries to nearby organs or structures, and medical complications such as blood clots or poor reactions to medications. Fortunately, not one of our patients has ever required a blood transfusion or had a serious surgical complication.
Risks specific to the tubal reversal include: (1) the small chance that neither tube can be repaired, (2) the chance that the tubes are successfully repaired but that a patient still has difficulty conceiving due to other forms of infertility, (3) the possibility of a tubal or ectopic pregnancy, and (4) the unlikely possibility that the tubes are repaired but do not remain open.
Tubal Ligation Reversal Recovery Time
The initial recovery time is approximately two weeks, but some patients report feeling 80-90% recovered in just one week. Most often, Dr. Lipskind will tell you that you are safe to return to work, drive a car, and start trying to become pregnant after your two week postoperative appointment. There are no physical restrictions after 6 weeks.
Getting Pregnant After Tubal Ligation Reversal
The average time to pregnancy after the surgery is about 6-7 months. Pregnancy may take longer if only one tube was able to be repaired since you can ovulate from either side any given month. In such cases, Dr. Lipskind may offer treatment with low dose fertility medications to improve the odds of ovulation on the side that was successfully repaired.
As soon as you are late on your period or have a positive home pregnancy test, you should notify ACFS so that we can send you an order for a blood pregnancy test (serum quantitative hCG). We will follow the rise in hCG to ensure that the levels are increasing normally and schedule you for your first ultrasound between 5-6 weeks’ gestation (usually within two weeks of your first positive pregnancy test). Once we confirm a viable pregnancy in the uterus, you can continue routine pregnancy care with your general OB/GYN.
Successful pregnancy depends on the age of the woman. Live birth rates range from 40% at age 40-42 to over 85% for women under the age of 35. Miscarriage risk is not increased as a result of the reversal surgery. If a couple is not successful in conceiving within 6 months after tubal reversal, we will recommend an x-ray, or HSG, to document tubal patency. Once the tubes are confirmed to be open, the couple can continue to attempt pregnancy naturally or expand their evaluations for other sources of infertility and start treatment for non-tubal infertility.
Reversal of Sterilization Vs. In Vitro Fertilization
In-Vitro Fertilization (IVF) is the main alternative to tubal ligation reversal. There are advantages and disadvantages for both treatment options. Since ACFS has a great deal of experience and excellent results with both surgery and IVF, we are in a unique position to provide an unbiased assessment of which treatment may be better for any particular couple. In the end, if patients are good candidates for either procedure, we feel strongly that it should be the patient’s choice—not ours—which guides her treatment.
Advantages for IVF include:
- No need for abdominal surgery and the associated risks and healing time.
- Addresses other forms of infertility, including sperm problems, ovulatory disorders, and the age-related increase in chromosomally abnormal conceptions with very high rates of success.
- No need for contraception after childbearing is complete.
- The potential to save fertility for future pregnancies through embryo cryopreservation.
- Lower risk for ectopic pregnancy.
- The option for gender selection, or family balancing, through IVF with PGT
Disadvantages for IVF include:
- Opportunities for children are limited by the number of eggs and healthy embryos that a woman produces with each attempt.
- Some couples prefer the idea of trying naturally (even when pregnancy chances are likely to be higher with IVF).
- Does not restore functional tubal anatomy for patients who “want to feel whole” again or who have symptoms possibly related to post-tubal ligation syndrome (PTLS).
The advantages and disadvantages of tubal ligation reversal are pretty much the inverse of the pros and cons for IVF.
Tubal Ligation Reversal Cost
We find that cost is frequently cited as a deciding factor for most couples who would be good candidates for either treatment. For many years, tubal reversal was regarded as being less expensive than IVF. Today these treatments are very close in price when comparing the surgery vs. a single IVF treatment. Most patients can therefore make a decision about the best treatment path for them based on their individual priorities and needs rather than cost alone.
Final Thoughts
If you’ve had a tubal ligation and are interested in tubal reversal surgery or IVF, what are you waiting for? We are experts in both of these treatments and have helped countless patients from Arizona and from out-of-state who were told that they would never be able to have children again. Call ACFS to schedule your consultation today.
Success Stories
If you want to learn more about tubal ligation reversals, call your ACFS fertility team today at (480) 860-4792.











