Polycystic Ovarian Syndrome (PCOS/PCOD)
What is Polycystic Ovary Syndrome (PCOS)?
Polycystic Ovary Syndrome (PCOS) is a common reproductive endocrine disorder characterized by ovulatory dysfunction, excess androgen hormone levels, and polycystic appearing ovaries on ultrasound.
Women with PCOS may have absent or irregular menstrual cycles, acne, excessive hair growth, and/or infertility.
Because of the variable nature of PCOS and overlapping symptoms with other disorders, the diagnosis of PCOS is based upon a combination of clinical, ultrasound, and laboratory features.
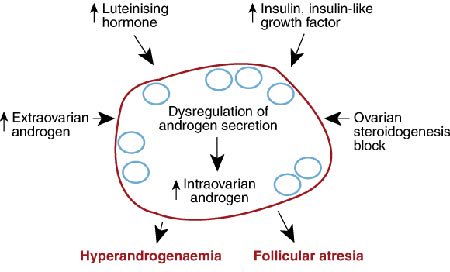
The pathophysiology of polycystic ovary syndrome. Large numbers of small, cyst-like ovarian follicles are resistant to normal growth signals and therefore are unable to release eggs. Luteinizing hormone (LH), androgen, and insulin levels may be elevated and can correlate with acne, excess hair growth, and abnormal blood sugar metabolism, or diabetes.

Ultrasound of a polycystic ovary containing multiple dark fluid-filled cysts.
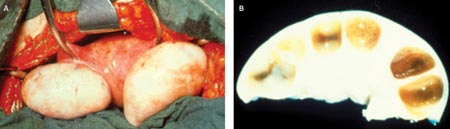
Surgical photos of PCOS ovaries, which are typically enlarged and have a smooth surface without any signs of recent ovulation (Photo A). Coss-section of a polycystic ovary reveals multiple cysts below the surface of the ovary (Photo B).
PCOS Risks Factors
PCOS and Metabolic Syndrome
Women with Polycystic Ovary Syndrome (PCOS) may be also at increased risk for developing a metabolic syndrome, which is characterized by abdominal obesity, cholesterol abnormalities, high blood pressure, and insulin resistance, which impairs blood sugar regulation.
For overweight women with PCOS, modest weight loss through diet and exercise can often lead to spontaneous ovulation and pregnancy.
PCOS and Type 2 Diabetes
Even normal-weight women with PCOS have an increased risk of developing Type 2 diabetes due to insulin resistance. Insulin resistance usually occurs before hyperglycemia, or increased blood sugar levels.
In addition to weight loss through diet and exercise, some anti-diabetic medications can be used to help promote ovulation in women with PCOS.
PCOS and Endometrial Cancer
Lack of ovulation in women with PCOS results in continuous exposure of their uterine lining (endometrium) to estrogen. This may cause excessive thickening of the endometrium and heavy, irregular bleeding.
Over many years, the continuous stimulation for endometrial growth without regular progestin-induced shedding of the lining can lead to precancerous changes in the lining of the uterus and possibly even endometrial cancer.
The good news is that there are several easy and commonly used options for endometrial protection, including the use of birth control pills and progestin-secreting IUDs. Inducing ovulation and becoming pregnant also have a protective effect.
Polycystic Ovary Disease (PCOS) Treatments
Dealing with PCOS can be emotionally difficult. Women with PCOS may worry about their ability to have children and feel self-conscious about their physical appearance.
Fortunately, there are a number of treatment options that can effectively reduce the side-effects of PCOS and help achieve pregnancy, depending on one’s individual goals.
If fertility is the immediate goal, clomiphene citrate (Clomid®) and letrozole (Femara®) are oral medications that are frequently used to induce ovulation. These may be combined with careful monitoring for ovulation and timed intercourse or intrauterine insemination.
Injectable gonadotrophins may be used to induce ovulation if the ovaries do not respond to oral medications, but they are more expensive and associated with a greater chance of multiple pregnancies.
Medications that increase the body's sensitivity to insulin, such as metformin (Glucophage®), may also lead to more regular ovulation.
Surgeries aimed at decreasing ovarian volume and ovarian androgen levels have also proven to be effective in increasing ovulation rates. These include ovarian wedge resection, diathermy, or ovarian drilling.
Due to the availability of less invasive treatment options and the risks of ovarian surgery (ovarian injury and scar tissue formation), these techniques are rarely recommended at ACFS.
If fertility is not an immediate concern, hormonal therapies are usually successful in temporarily correcting the problems associated with PCOS.
Oral contraceptive pills (OCPs) are commonly prescribed to reduce acne and unwanted hair growth, maintain regular menstrual periods, prevent endometrial cancer, and prevent unintended pregnancy.
Vaniqa®, spironolactone, electrolysis and laser hair removal can also be helpful for reducing the appearance of excess facial and body hair.
Request Your Consultation Today!
If you want to learn more about polycystic ovary syndrome (PCOS), call your ACFS fertility team today at (480) 860-4792.
Sources:
The American Society for Reproductive Medicine











