Never Do a Day 3 Embryo Transfer
Published: 12/15/2015
At the Arizona Center for Fertility Studies we’ve researched for years, and demonstrated that if your embryos were not able to reach the blastocyst stage (day 5) in ACFS-ART laboratory culture system and were transferred at an earlier stage (day 3), they would not have survived in utero. The same is true of frozen embryos. If they do not survive the freeze/thaw process (vitrification) at ACFS, then they would not have survived in a fresh transfer.
Some clinics disagree with these conclusions, but our experience supports them. We abandoned the routine use of day 3 embryo transfer several years ago and our patients have seen higher success rates since. This shift would not have been possible were it not for our ability to safely and reliably culture embryos to day 5 or 6, then freeze and thaw those embryos with extremely high survival rates. Some clinics still do day 3 transfer because they are not comfortable with growing embryos out to day 5-6 (advanced blastocyst culture) or tell their patients "it is better to transfer on day 3" because “the uterus provides a better environment for the embryo” than the lab. Our ACFS team respectfully disagrees. We believe it is more cost effective to see if the embryos make it to day 5. If embryos arrest in development prior to reaching the blastocyst stage, they are almost always chromosomally abnormal. We are therefore confident that they would not have survived in the uterus either, and that it is kinder and more cost-conscious to save patients the emotional and financial expense of embryo transfers that are doomed to fail.
One of the principal reasons In Vitro Fertilization (IVF) fails is that the embryo(s) do not implant in the uterus after transfer. Numerous modifications and advancements in the IVF culture media —like blastocyst culture and chromosome testing or PGS — can now improve chances of implantation.
Many embryos transfers are done on day 3 after egg collection in a fresh cycle. Some embryos do well in culture, while others do not. It’s hard to tell which type of embryos you have. If embryos are cultured in the laboratory for a longer period of time (day 5-6), they may develop further to the blastocyst stage. At this stage the embryo has already differentiated and is made up of more than 100 cells, enabling us to identify groups of cells that will make up the placenta (trophectoderm cells) and the fetus (stem cells) or what’s called the ICM or inner call mass.

A nice looking day 5 blastocyst with an ICM, inner cell mass or stem cells, a blastocyst cavity (C) and a ring of outer cells, known as trophectoderm, that will develop into the future placenta.
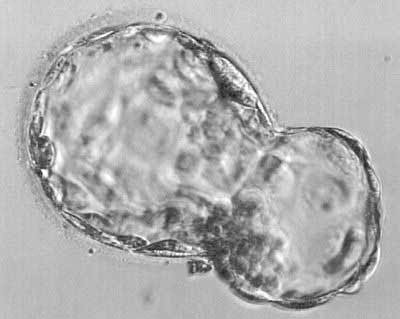
Picture of a very nice looking day 6 "hatching" blastocyst. This is where the blastocyst begins to break out of its shell (zona pellucida), getting ready for implantation on cycle day 6-1/2 from fertilization.
Growing embryos in the laboratory is a difficult process. The longer they remain in culture the greater the chance that some or all of the embryos produced by the In Vitro Fertilization (IVF) process will not survive. That’s the argument some clinics try to make. At ACFS, we’ve repeatedly observed the opposite. We believe, that in an excellent IVF laboratory with an experienced and skilled embryologist, many embryos do survive to day 5-6 or the blastocyst stage and have a greater chance of implanting. We were not able to say this 5-6 years ago, but after much research and observation we can confidently claim that if your embryos were not able to reach the blastocyst stage (day 5) in ACFS-ART laboratory culture system, they would not have survived in utero were they transferred at an earlier stage (day 3).
Here’s what enabled our mastery of this new technology:
First, ACFS was driven to be successful on each patient’s first attempt at IVF (for obvious reasons).
Second, with the new PGS technology that enabled us to test each embryo’s chromosomes, we had a number of biopsied day 3 embryos that made “beautiful” day 5 embryos or blastocysts, but came back chromosomally abnormal. At the time, there was no scientific evidence supporting the speculation that embryos could “self-correct”. With patients’ permission and informed consent, we asked to re-biopsy these abnormal day 5 blastocysts to see what percentage of them, if any, had “self-corrected”. In collaboration with 3 other clinics we found that in the first 24 days, 5-6 embryos re-biopsied, 64% had “self-corrected” and were read as normal. ACFS, along with 3 other major clinics, published what we believed at the time to be the first scientific paper demonstrating that embryos could “self-correct” by day 5-6 of development. That was the last time ACFS did day 3 embryo transfers or biopsies. This changed propelled our team to become proficient in culturing embryos out to the blastocyst stage.
New and advanced blastocyst culture methods significantly improved our ability to grow embryos to the blastocyst stage. Said differently, only the "best of the best" embryos make it to the blastocyst stage. Since blastocysts are "very good embryos" they tend to freeze and thaw very well. On the other hand, good day 3 embryos also freeze and thaw well. However, for the last 5-6+ years, we have cultured all of our patients’ embryos to the blastocyst stage with excellent results. We can say with confidence, that if your embryos do not make it to day 5-6 in ACFS in-vitro culture environment, they would not have been successful even if transferred on day 3. Since only the “best of the best” make it to the blastocyst stage, this is very important information to consider.
By not waiting to see whether or not day 3 embryos can make it to the blastocyst stage, you may be saving yourself the cost and heartbreak of multiple failed transfers. Obviously, some day 3 embryo transfers are successful, however, in our opinion, they would have progressed to day 5-6 anyway. Unfortunately, there is no way to predict these odds in advance.
Some fertility specialists believe that the uterus is the natural and “superior” environment to the IVF laboratory. Our team at ACFS respectfully disagrees, and strongly feels that in our culture system patients of all ages can successfully develop good embryos to the blastocyst stage. And if they do not, they would not have been successful if transferred on day 3. Based on our extensive experience with embryo culture, we strongly recommend growing all embryos to the blastocyst stage (day 5). The Arizona Center for Fertility Studies consistently achieves much higher pregnancy rates with a day 5 blastocyst transfer.
Every couple considering these procedures should be aware that there have been a few animal studies that raised concerns about neonatal problems such as increased birth weight and fetal abnormalities. There is no evidence at the present time of similar problems following the transfer of human blastocysts.
Our years of success with 23-chromosome microarray along with our conclusive evidence that embryos can "self-correct", enables us to confidently recommend growing all embryos to the blastocyst stage and doing chromosome testing or PGS on all day 5-blastocysts using laser-directed TE (trophectoderm) biopsy techniques. This means that after the blastocyst is biopsied, it will undergo cryopreservation and be transferred in a subsequent or following cycle. Although this obligates the couple to wait a cycle before doing the transfer, we want to offer them the following advantages of growing embryos to the blastocyst stage and doing chromosome testing or PGS (as opposed to a day 3 embryo transfer or day 3 embryo biopsy):
- It eliminates dealing with the possibility of "self-correction", which we’ve observed is more common than expected. ACFS was in a unique position to be able to re-biopsy normal-appearing day 5-6 blastocysts at no charge. Most clinics are not able to do this. If they’re doing day 3 embryo transfer and/or biopsies and the chromosomes come back abnormal, they have to discard the embryos because without re-biopsy there is no way to know if they "self-corrected" and it’s too risky to just assume they did. We strongly recommend day 5-6 TE biopsy for PDG/PGS with subsequent FET, so couples will never have to worry about discarding "normal" embryos.
- Another reason to culture embryos out to day 5-6, then do chromosome testing or PGS, is that there is evidence to suggest that embryos do better when left in group culture through the blastocyst stage than they do when separated on day 3 during a day 3 embryo transfer and/or biopsy.
- Additionally, day 3 biopsy has an increased chance of failed amplification (see below) because only one cell is being removed. With a blastocyst or TE biopsy you can safely remove 3-4 cells, which eliminates the risk of failed amplification and gives a more accurate interpretation for chromosome testing or PGS.
- Also, the blastocyst culture and cryopreservation, with subsequent FET, enables the patient to be stimulated more aggressively to make more eggs/embryos, and to be triggered with Lupron, rather than with hCG hormone. This significantly reduces the risk of ovarian hyperstimulation syndrome (OHSS).
- Finally, a couple only pays for embryo transfer if the embryos reach the blastocyst stage and/or come back chromosomally normal. A day 3 embryo transfer and/or biopsy require all embryos to eventually undergo a transfer and/or biopsy (because we don’t know which ones will develop into blastocysts). When growing all embryos to day 5-6, if the embryos do not reach the blastocyst stage (very unlikely at ACFS), at least you’re not paying for possible multiple embryo transfers and/or chromosome testing of embryos that could not survive past day 3 or the cleavage stage.
- We realized that frozen embryo transfers were producing 30% higher pregnancy rates and significantly reduced the risks of ovarian hyperstimulation syndrome (OHSS). This allowed our team to use more aggressive stimulation protocols, which helped recover increased quality and quantity of eggs with resulting higher numbers of “quality” embryos for transfer and more remaining to cryopreserve.
We’ve seen all these advantages collectively produce higher success rates. This is why we now strongly recommend growing all embryos to the blastocyst stage, doing PGS, cryopreservation, and subsequent next cycle frozen embryo transfer or FET.
Five years ago we stopped doing day 3 transfers — with or without chromosome testing. Because only the "best of the best" embryos make it to day 5, those embryos that do not make it to the blastocyst stage (stage 5), are not biopsied, saving the patient the anxious wait for day 3 biopsy results, as well as a considerable amount of money by avoiding unnecessary transfers.
At ACFS, we excel at good day 5 blastocysts, even in reproductively older women. We’re able to control the entire process: ovarian stimulation (COH), fertilization using ICSI, blastocyst culture, developing the embryos to day 5, the freeze-thaw process (vitrification), and uterine transfer. Of course we cannot control whether or not the embryos are chromosomally normal. That’s why we’ve adopted the "If you can’t control it, maximize it" strategy.











